Ask Dr Iain-Aetiology

Ned having a blood glucose reading from a blood drop extracted from next to a toe pad. Is he really diabetic?
Ask Dr. Iain- Aetiology!
Can epilepsy, diabetes and cancer / tumours be hereditary in dogs?
Regards Jackie Gauci
Aetiology (pronounced, eight-tea-ology, at least that’s how I pronounce it!) is a word that describes the causes of a disease. Essentially the question is whether cancer, tumours, epilepsy and diabetes can have a hereditary aetiology in dogs.
The brief answer is yes; there very well may be in many cases. Each disease mentioned could warrant pages of discussion on their various causes but in virtually all cases your vet will probably say that there is a breed susceptibility to each disease which doesn’t always mean that there has been a particular genetic defect or mutation identified as the cause. In fact, it is very rare that a genetic cause has yet been identified for most cases of these diseases despite there being many definite breed susceptibilities.
Another complication is that for each disease listed there can be dozens of forms of the disease, each with specific causes or unknown causes with or without a known breed susceptibility. It can become very complicated especially when two people discussing say, epilepsy, might be talking about two different types of diseases that cause fits/seizures without realising it.
Fortunately, Griffons aren’t particularly susceptible for all of these diseases.
Epilepsy is best described as a chronic disease that involves recurrent seizures (fits). Not all seizures are caused by epilepsy. If a dog suffers a fit, the vet will usually determine with the help of clinical history, examination, blood tests and sometimes further testing, if there is some other cause rather than epilepsy that is responsible. A complication is that some vets refer to ‘other causes’ of fits as secondary or symptomatic epilepsy, which I don’t think is very helpful! Some causes of fits that aren’t epilepsy are,
-Ingestion of a poison or trauma to the head,
-Insulinoma, a pancreatic tumour producing excessive insulin and causing low blood glucose levels that can trigger fits.
-Brain infection due to virus, bacteria or parasite.
-Porto-systemic shunts (where there is an abnormal blood vessel that by-passes the liver so that blood flowing from the intestines containing bacterial toxic metabolites from the gut is not ‘cleansed’ by the liver before reaching the heart. This means that the brain will receive excess toxins following a meal, which in turn can cause a fit).
-Brain neoplasia (cancer/tumour), especially in an older dog and may require scans being carried out at a Specialist Centre to diagnose. Blood tests often will appear normal.
These are just a few examples of other causes of fits occurring in dogs. If initial tests are negative and especially if the dog is between say 2 to 5 years of age and further fits occur, then most vets will diagnose ‘epilepsy’ (aka primary or idiopathic (unknown cause) epilepsy). Do we know the actual cause of epilepsy in most of these cases? No, but we might speculate that there was a brain injury due to lack of oxygen during birth or discuss that there might be a genetic cause especially if the breed is one where cases are more frequently seen like the Belgian and German Shepherd, Cocker Spaniel, St Bernard, Golden or Labrador Retriever amongst others.
Does not knowing the cause of epilepsy make any difference to the treatment? No, the medications used are the same and usually involve phenobarbitone tablets and occasionally potassium bromide, if the fits are severe or are occurring frequently enough to warrant treatment. There is no genetic test for epilepsy currently available but there is much research being carried out attempting to find genetic markers in various breeds. An example is the Belgian Shepherd (Tervuren) where genes have been identified that seem to be linked to those affected by epilepsy. As yet there is no commercial test available to distinguish between those Belgian Shepherds who will have epilepsy (carrying a pair of ‘epilepsy’ genes) and those who are carriers (carrying a single ‘epilepsy’ gene but not affected) and those who don’t carry the genes at all, assuming it is a genetic recessive disease. Ideally we would select those not carrying the causative genes or at least mate a carrier with another not carrying the responsible gene for breeding.
Diabetes is a name given to two very different diseases. The very rare one is diabetes insipidus (water diabetes) and the far more common one that we are usually referring to is diabetes mellitus (sugar diabetes).
We all know that diabetes mellitus occurs when the pancreas is producing insufficient insulin which is a hormone needed by cells throughout the body to absorb glucose from the bloodstream for metabolism. People can either have type 1 diabetes, usually diagnosed in children and young adults, where there are insufficient pancreatic insulin producing cells, or type 2 diabetes which is more common in older patients who for various reasons including obesity can become resistant to the insulin they are still producing.
When dogs get diabetes, they are more akin to type 1 human diabetic patients, i.e. they always need insulin injections for the rest of their life. Cats usually are more akin to type 2 human diabetic patients in that they may need insulin initially but if fed an appropriate diet and possibly lose any excess weight they may eventually be cured and no longer require insulin injections.
Aetiology of canine diabetes? Usually we don’t know the cause and even in cases where we do know the cause it makes no difference to the treatment, virtually all canine patients need insulin injections and control is best helped by a regimented low carbohydrate diet, regimented exercise and ideally regular at home blood glucose testing.
Sometimes, if the patient has had known episode/s of pancreatitis (see Ask Dr Iain-Pancreatitis on our Club’s website!) then we can attribute the diabetes to pancreatic destruction. If too much of the pancreas has been destroyed then there will be too little insulin producing cells left to produce adequate insulin. Many of these dogs will have chronic diarrhea due to loss of pancreatic digestive enzyme production and will need both insulin injections and digestive enzymes added to their food.
Another cause is where diabetes is a result of having Cushing’s disease (hyperadrenocorticism) where high blood levels of cortisol that result from this disease are antagonistic to insulin. Sometimes being able to treat the Cushing’s disease successfully will mean the patient no longer needs insulin injections. Similarly, the higher levels of progesterone in pregnant dogs can cause gestational diabetes as can occur with pregnant women.
However, in most cases of diabetes we don’t know the exact cause (i.e. idiopathic) but there is certainly breed susceptibility that indicates a genetic component. Some susceptible breeds include, Border Collies, Samoyed, Schnauzers, Keeshond, Puli, Poodles, Beagles, Tibetan Terrier, Dachshunds and Cairn Terrier, amongst others. There is also a very rare congenital form of diabetes that has been documented in Keeshonds and Labradors that can affect very young dogs under 12 months of age.
To add another layer of complexity is the fact that type 1 diabetes in people also occurs more frequently in some families, which is not dissimilar to the situation in dogs where we might consider different breeds of dogs as genetically similar families. However, type 1 diabetes is also shown in people to have a immune mediated component, where one’s own immune system is actually destroying the insulin producing cells of the pancreas, and many human type 1 diabetic patients will have other autoimmune or immune mediated diseases. I should know, as I’m a type 1 diabetic myself with other immune mediated diseases! The same situation seems to occur in dogs. So, the genetic basis to diabetes might actually be towards developing immune mediated diseases. Let me add another layer of complexity; many years ago I played in an orchestra (I’m an undistinguished violinist) where another member (a trombonist) was a diabetes research scientist. He was working on proving that exposure to a virus that infects potatoes can trigger diabetes in people, i.e. virus exposure triggering an immune response that induced destruction of pancreatic insulin producing cells leading to type 1 diabetes. It could be a genetic susceptibility in some patients allows this to occur. So, although there is breed susceptibilities it may not always mean that carrying a particular gene will directly cause diabetes, it may actually indirectly cause it due to increased risk of developing an immune mediated disease that can be triggered by exposure to something else like a virus!
As yet there are no genetic tests available to predict diabetes in dogs. Should we prevent our dogs from eating potatoes? No, but just as it applies to us, don’t let them eat the toxic green ones!
Let’s pretend that Ned is a diabetic and is owner is giving him two insulin injections daily, each a 1/2 hour before his morning and evening meal. Ned has had a regular blood glucose test before his insulin injection. This is done using the spring loaded lancet to get a drop of blood to test with the glucometer from either his inside upper lip or just to the side of a footpad. The footpad is easier with brachycephalic dogs or those that might bite! (see picture at start of article)
These are three readings that Ned might have, (a), (b) or (c)!
(a) (b)
(b)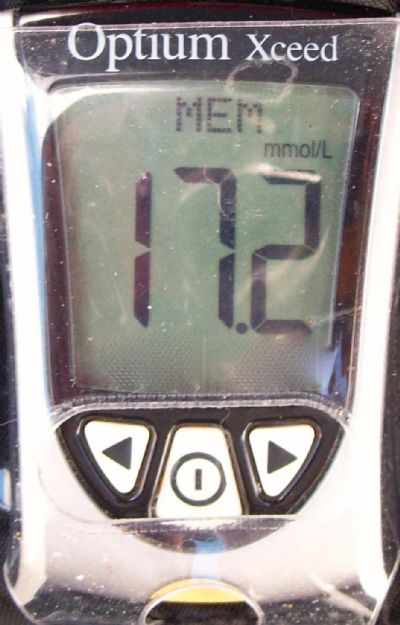 (c)
(c)
What should we do with his insulin dose in each case? (answers at the end of the article!)
Cancer/neoplasia/tumours are interchangeable terms describing the same group of diseases, which can affect any organ or tissue throughout the body. There are malignant cancers, which can spread to other organs and tissues from where they arise, and benign cancers, which don’t spread via the blood or lymphatic systems from where they arise but can sometimes be locally very invasive.
The list of causes is too numerous to properly discuss here but some causes are well established in dogs as they are in people. Exposure to excessive UV radiation can cause melanoma and cutaneous haemangiosarcoma in dogs, especially fair skinned dogs that like to sunbake while lying on their backs.
Similarly, exposure to cigarette smoke can cause lung cancer in dogs as can exposure to other carcinogens. Being left entire (i.e. not being spayed) does increase the risk of mammary cancer in bitches as they get older due to ongoing mammary gland exposure to progesterone, however, being spayed or neutered/castrated (in the case of male dogs) before reaching full physical maturity does increase the risk of developing some other forms of malignant cancer as well as some orthopedic conditions such as ruptured cruciate ligaments and hip dysplasia later in life. This is why more vets are recommending delaying desexing surgery until the dog or bitch is physically mature, i.e. at least 12 months of age for smaller dogs.
However, like the diseases already discussed, there are many known breed susceptibilities to various cancers and with time there will probably be many causative genes identified that may be able to be identified with commercial DNA-tests.
So far there is only one DNA-test available that tests for a hereditary aetiology cancer in dogs, i.e. renal cystadenocarcinoma and nodular dermatofibrosis, which respectively affect the kidneys and skin of affected German Shepherds. There are many other genetic diseases that aren’t cancers for which DNA testing is available but fortunately none of these diseases are prevalent in Griffons. We are hoping that some time in the future, a DNA test night become available for SM/CM (Syringomyelia/Chiari-like Malformation), which is prevalent in Griffons.
The Griffon Bruxellois is fortunately not found among those breeds with known susceptibilities to cancers such as Golden Retriever (lymphoma), Boxers and Pugs (multiple mast cell tumours), Scottish Terriers (transitional cell carcinoma of the bladder) and numerous others. However, there is much promising research aimed at identifying genes that could be responsible for cancer in various breeds, especially lymphoma, haemangiosarcoma and osteosarcoma, and there is no doubt that DNA testing will become available for more cancer causative genes as years go by.
Answers to the Diabetes Quiz.
(a)  This is a perfect reading (between 5-10mmol/l blood glucose). We wouldn’t change anything and would give his usual insulin injection.
This is a perfect reading (between 5-10mmol/l blood glucose). We wouldn’t change anything and would give his usual insulin injection.
(b) 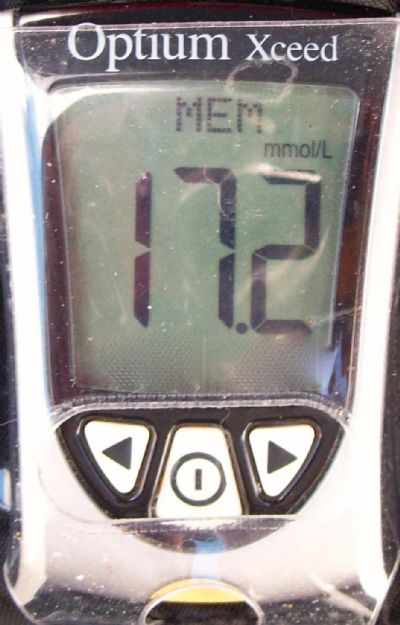 This reading is too high (hyperglycaemic) but we wouldn’t increase his insulin dose without confirming that the high reading might be due to a Somogyi effect. To do that we would take another reading, say 4 hours after his insulin dose and meal. If this reading is also high then we would increase his subsequent insulin doses, but if this reading were low then we would be confirming that we have a Somogyi effect where the dose of insulin is actually too high and causing a hypoglycaemic episode. After a ‘hypo’ the body will release excess glucose from the liver and we’ll see a high reading a few hours later. In this case we would actually lower the subsequent insulin doses. If a patient is having a Somogyi effect and we increase the insulin after recording a high rebound glucose reading, we actually will make the situation worse and risk an even more severe hypoglycaemic episode. This situation is very common even with human diabetics. Yes, this was a trick question!
This reading is too high (hyperglycaemic) but we wouldn’t increase his insulin dose without confirming that the high reading might be due to a Somogyi effect. To do that we would take another reading, say 4 hours after his insulin dose and meal. If this reading is also high then we would increase his subsequent insulin doses, but if this reading were low then we would be confirming that we have a Somogyi effect where the dose of insulin is actually too high and causing a hypoglycaemic episode. After a ‘hypo’ the body will release excess glucose from the liver and we’ll see a high reading a few hours later. In this case we would actually lower the subsequent insulin doses. If a patient is having a Somogyi effect and we increase the insulin after recording a high rebound glucose reading, we actually will make the situation worse and risk an even more severe hypoglycaemic episode. This situation is very common even with human diabetics. Yes, this was a trick question!
(c)  This reading is too low and Ned is actually having a hypoglycaemic episode and he may even be weak, shaky, panting, confused and if left untreated he may even become unconscious. With a hypoglycaemic reading we would immediately give him some glucose syrup or honey or even a few jelly beans if he would eat them. After retesting his blood glucose and ensuring it had normalised, we would immediately lower the next insulin dose and then give him his normal meal. After a ‘hypo’ it is always appropriate to lower the insulin dose and we don’t need to see if another reading is low before doing so.
This reading is too low and Ned is actually having a hypoglycaemic episode and he may even be weak, shaky, panting, confused and if left untreated he may even become unconscious. With a hypoglycaemic reading we would immediately give him some glucose syrup or honey or even a few jelly beans if he would eat them. After retesting his blood glucose and ensuring it had normalised, we would immediately lower the next insulin dose and then give him his normal meal. After a ‘hypo’ it is always appropriate to lower the insulin dose and we don’t need to see if another reading is low before doing so.
Iain Mitchell BVSc(Hons), MANZCVSc.
Contact Details
President: Mrs Colleen De Haan [email protected]
Secretary -Mrs Robin Simpson [email protected]
Puppy enquiries - Beth Canavan [email protected]
0490085215